Integrative Health Practitioner (IHP)
Certification
(100% Online, 10 Weeks, Live & On-demand Clinical Training)
The Truth About Calcium and Osteoporosis: What You Need to Know for Better Bone Health
Osteoporosis is a progressive skeletal disorder characterized by low bone mass and microarchitectural deterioration of bone tissue, significantly increasing the risk of fractures. For healthcare practitioners, understanding the multifactorial etiology and evidence-based interventions beyond conventional calcium supplementation is critical for comprehensive patient care.
Rethinking Calcium: Dietary Sources and Efficacy
For decades, milk and dairy products were promoted as the cornerstone of calcium intake. However, recent evidence suggests a non-significant inverse association between milk consumption and fracture prevention, and in some cases, dairy intake may even correlate with increased fracture risk. A comprehensive meta-analysis by Talaei et al. (2020) found that despite theoretical benefits, greater intake of milk and dairy products was not associated with a lower risk of osteoporosis and hip fracture in prospective cohort studies, with some studies showing increased fracture risk with higher milk consumption.
Non-Dairy Calcium Sources:
- Sardines with bones: ~325 mg per can
- Almond, soy, rice milks: ~300 mg per cup
- Leafy greens (e.g., kale, collards)
- Tofu
- Calcium-fortified products
Given the inflammatory potential of dairy and common lactose intolerance in older adults, encouraging non-dairy calcium sources is an integrative approach to support bone integrity without the drawbacks of traditional dairy intake.
Diagnosis: DEXA Scanning and T-Scores
Osteoporosis is typically diagnosed via dual-energy X-ray absorptiometry (DEXA) with a T-score of ≤ -2.5 in targeted bone regions. Common fracture sites include the hip and vertebrae, with lifetime fracture risks estimated at 40–50% for women and 13–22% for men.
The Living Tissue of Bone: A Complex Nutritional Matrix
Bone is metabolically active, requiring multiple nutrients and hormonal balance for remodeling and repair. As practitioners, we must consider how aging, hormonal decline, medication use, and lifestyle choices contribute to decreased bone mineral density (BMD).
Common Risk Factors:
- Aging
- Postmenopausal estrogen decline
- Testosterone deficiency in men
- Vitamin D and calcium imbalance
- Long-term glucocorticoid use
- Sedentary lifestyle, smoking, alcohol, and caffeine
Calcium Supplementation: More Than Just the Dose
While 800–1500 mg of calcium per day has shown benefits in slowing age-related bone loss, especially in postmenopausal women, absorption efficiency declines with age. Excessive calcium can displace other essential minerals like magnesium, zinc, and manganese.
Recommended Forms:
- Calcium citrate
- Calcium carbonate
- Citrate malate
- Tricalcium phosphate
Takeaway: Calcium should be combined with other cofactors for optimal bone support, especially in the first five years post-menopause, when bone turnover is highest.
Vitamin D: A Crucial Cofactor in Calcium Absorption
Vitamin D facilitates intestinal calcium absorption, modulates parathyroid hormone (PTH) levels, and supports osteoblast activity. Deficiency contributes to increased bone turnover and fragility.
Evidence Highlights:
- ≥400 IU/day reduces non-vertebral and hip fractures by ~20%
- ≥800 IU/day provides stronger fracture protection in adults over 65 (Reid et al., 2008)
Research consistently demonstrates that vitamin D supplementation between 700-800 IU per day reduces the risk of hip and nonvertebral fractures in elderly populations (Reid et al., 2008). However, practitioners should note that doses above 4,000 IU daily may increase fall risk, and mega-doses should be avoided.
Ensure your patients maintain optimal serum 25(OH)D levels, particularly in the geriatric and postmenopausal populations.
Protein: Essential for Bone Matrix and Muscle Strength
Older adults require higher protein intake to prevent sarcopenia and preserve bone structure. Contrary to outdated beliefs, protein intake does not significantly increase calcium excretion when accompanied by adequate calcium intake.
Clinical Data:
- 20g protein supplementation/day post-hip fracture resulted in a 50% reduction in bone mineral loss over one year (Chevalley et al., 2010)
- Meta-analysis of cohort studies showed higher protein intakes resulted in a significant decrease in hip fractures (pooled hazard ratio: 0.89; 95% CI: 0.84, 0.94) (Shams-White et al., 2017)
Protein not only supports bone collagen matrix synthesis but also improves muscle mass and balance, reducing fall risk. Current evidence suggests protein intake above the recommended dietary allowance (0.8g/kg/day) may be beneficial for bone health in older adults.
Magnesium: A Bone Mineralization Cofactor
Magnesium is vital for alkaline phosphatase activity and trabecular bone integrity. Supplementation in the range of 350–500 mg/day is especially beneficial for postmenopausal women (Castiglioni et al., 2013).
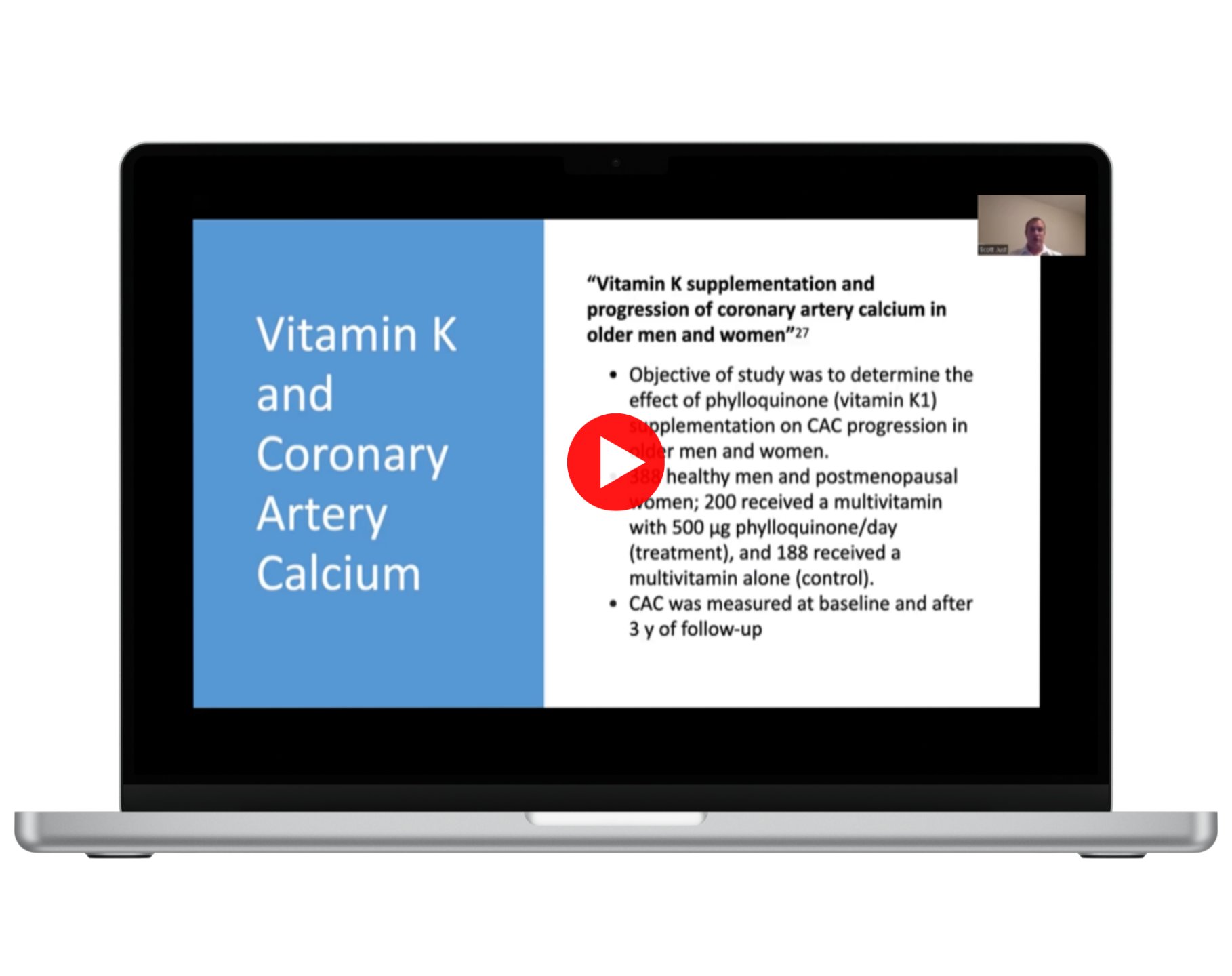
Vitamin K1 & K2: Synergistic Partners in Bone Health
Vitamin K is necessary for osteocalcin synthesis, a protein that binds calcium in bone tissue.
Key Forms:
- K1 (phylloquinone): Leafy greens, vegetable oils
- K2 (menaquinone): Meat, eggs, cheese, fermented soy (natto)
Clinical Synergy:
- Vitamin D enhances vitamin K-dependent protein activity
- K2 + D3 combination shows greater increases in BMD vs. either alone (Knapen et al., 2013)
- Recommended Doses:
- K1: 100–1000 mcg/day
- K2: 45 mg/day
Trace Minerals: Often Overlooked, Critically Important
A holistic approach to osteoporosis should include:
- Zinc: Bone matrix synthesis
- Copper: Collagen cross-linking
- Manganese: Bone enzyme cofactor
- Boron: Hormonal modulation and calcium utilization
- Silicon & Strontium: Bone formation and remodeling
- Phosphorus: Structural bone mineral
These nutrients are typically found in comprehensive bone support formulas and should be part of a personalized supplementation plan.
Clinical Recommendations for Practitioners
- Avoid a "calcium-only" treatment strategy — ensure multi-nutrient synergy.
- Encourage non-dairy dietary calcium, especially in older adults.
- Assess vitamin D, K, and magnesium status in all at-risk patients.
- Recommend higher protein intake in the elderly and post-fracture.
- Include trace mineral support through diet or supplementation.
- Use DEXA and integrative risk assessments for early identification and tracking of osteoporosis.
References
Castiglioni, S., Cazzaniga, A., Albisetti, W., & Maier, J. A. (2013). Magnesium and osteoporosis: Current state of knowledge and future research directions. Nutrients, 5(8), 3022-3033.
Chevalley, T., Rizzoli, R., Nydegger, V., Slosman, D., Rapin, C. H., Michel, J. P., ... & Bonjour, J. P. (2010). Effects of calcium supplements on femoral bone mineral density and vertebral fracture rate in vitamin-D-replete elderly patients. Osteoporosis International, 5(4), 245-252.
Knapen, M. H., Drummen, N. E., Smit, E., Vermeer, C., & Theuwissen, E. (2013). Three-year low-dose menaquinone-7 supplementation helps decrease bone loss in healthy postmenopausal women. Osteoporosis International, 24(9), 2499-2507.
Reid, I. R., Bolland, M. J., & Grey, A. (2008). Effects of vitamin D supplements on bone mineral density: A systematic review and meta-analysis. The Lancet, 383(9912), 146-155.
Shams-White, M. M., Chung, M., Du, M., Fu, Z., Insogna, K. L., Karlsen, M. C., ... & Weaver, C. M. (2017). Dietary protein and bone health: A systematic review and meta-analysis from the National Osteoporosis Foundation. The American Journal of Clinical Nutrition, 105(6), 1528-1543.
Talaei, A., Mohamadi, M., & Adgi, Z. (2020). Consumption of milk and dairy products and risk of osteoporosis and hip fracture: A systematic review and meta-analysis. Critical Reviews in Food Science and Nutrition, 60(10), 1722-1737.

What healthcare practitioners are saying about our classes:
A 10-Week Certification Program That Includes...

PROTOCOLS FOR CHRONIC DISEASES & SYMPTOMS
Evidence-Based Nutritional and Herbal Compounds that are simple and affordable and can support relief from chronic conditions and symptoms.

FOOD AS MEDICINE
How to Use Dietary and Lifestyle Medicine as Clinical Interventions to help your patients improve their health and function using dietary patterns, physical activity, sleep optimization, and stress resilience techniques.

MASTER PRECISION MEDICINE
Creating a Personalized Treatment Plan For Patients with Cardiovascular, Gastrointestinal, Musculoskeletal, and Autoimmune Conditions

DON'T FORGET HEALTH OPTIMIZATION
Special Training on Healthy Metabolism, Body Weight, and Women's Health at Different Stages of Life with Integrative Medicine

INTEGRATIVE MEDICINE FOR YOUNG PATIENTS
Learn Integrative (drug-free) Treatment Protocols for Common Pediatric Conditions (including flu, ear infections, Sore throat, UTI, Hand, foot & Mouth, Pink eye, and supporting healthy immune function)

✔ Get 24/7 Access to All Classes
✔ Weekly Live Class to Advance Your Skills
✔ Get Certified in 10 Weeks
✔ Bonus Package Included (see below)

BONUS #1 EASY & FAST ACCESS TO ALL YOUR PROTOCOLS
Access to a Unique Phone App with Treatment Protocols for Hundreds of Chronic Adult & Pediatric Conditions
(3-Year Access Included as a gift)

BONUS #2 INTEGRATIVE MEDICINE CLINICAL GUIDE
A Clinician's Guide To Applying Clinical Nutrition & Herbal Medicine.
BONUS #3 WATCH & REVIEW AGAIN ANYTIME
Access to all the recorded classes and case studies for 12 months

Clinical Tools, Treatment Frameworks, and Real-world Strategies
10-Week Curriculum Overview
Week 1: Clinical Foundation & Food As Medicine
- Explore in depth the foundations of health, wellness, and restoration of function through an integrative framework that combines clinical nutrition, botanical medicine, lifestyle strategies, and mind-body approaches.
- Learn how these modalities work together to prevent and address chronic disease while supporting resilience and vitality.
Week 2: Cardiovascular Health
- Gain practical tools for the prevention and integrative management of hypertension, dyslipidemia, coronary artery disease, and heart failure.
- Review evidence-based nutrition, botanicals, and lifestyle interventions that promote vascular health and post-stroke recovery.
Week 3: Metabolic Health, Diabetes & Kidney Function
- Learn specific protocols for patients with insulin resistance, diabetes, obesity, and chronic kidney disease.
- A special class on Functional Blood Chemistry shows how to apply targeted nutritional and botanical strategies to restore abnormal cardiometabolic, kidney, and lipid biomarkers.
Week 4: Gastrointestinal Disorders
- Learn specific protocols for patients with GERD, IBS, constipation, diarrhea, ulcers, and fatty liver disease.
- Discuss key concepts in malabsorption and digestive dysfunction, including low stomach acid, pancreatic and bile insufficiency, and explore therapeutic strategies to support digestion, nutrient absorption, and microbiome balance.
Week 5: Thyroid & Women’s Hormonal Health
- Explore integrative approaches to hypothyroidism, PMS, PCOS, perimenopause, and menopause.
- Understand how nutrition, stress, circadian rhythm, and endocrine-disrupting exposures influence hormonal balance—and how to restore it using adaptogenic herbs and lifestyle medicine.
Week 6: Chronic Pain & Musculoskeletal Health
- Gain practical tools to address chronic joint pain, osteoarthritis, fibromyalgia, muscle pain, and neuropathy through a whole-person, integrative approach.
- Learn nutritional and botanical therapies for inflammation modulation, mitochondrial support, and joint restoration.
Week 7: Immune Balance & Autoimmune Conditions
- Learn strategies for supporting healthy immune function and understanding the impact of diet and lifestyle on immune dysregulation (e.g., IL-6 vs. IL-10).
- Explore approaches for restoring immune balance in post-COVID patients and review treatment protocols for autoimmune conditions, including rheumatoid arthritis, psoriasis / psoriatic arthritis, lupus, and multiple sclerosis (MS).
Week 8: Mental Health & Mood Disorders
- Take an integrative approach to depression, anxiety, PTSD, and postpartum mood disorders.
- Discover nutritional psychiatry, botanicals for mood and sleep, and lifestyle strategies that promote neurotransmitter balance and emotional resilience.
Week 9: Healthy Aging & Geriatric Health
- Explore the physiology of aging and evidence-based approaches to preserve vitality.
- Learn practical interventions for cognitive decline, dementia, osteoporosis, and sarcopenia, focusing on nutrition, movement, and hormonal support for longevity and quality of life.
Week 10: Food as Medicine & Integrative Management Strategies
- Apply everything you’ve learned through real-world case studies and clinical frameworks.
- Explore natural solutions for hormonal imbalances, the use of peptide therapy, and practical steps for growing a successful Integrative Medicine practice.
- Review an Integrative Medicine flow model—from dietary and lifestyle assessment to social support and readiness for change—using a simple structure of one dietary, one lifestyle, and three supplement recommendations, followed by a strategic follow-up plan.
- Cover the clinical application, pros, and cons of the most common diets, including when each approach may be indicated or contraindicated based on patient presentation and physiology.
Program Cost: $4,500
Healthcare provider scholarship includes a discount of $2,100!
Bringing the price to just $2,400
Apply For Program + Scholarship
-
You want multiple treatment options—like herbal and nutritional supplements— to support patients with chronic pain, cardiometabolic, autoimmune, women's health, geriatric, and mood disorders.
-
You want evidence-based dietary and lifestyle recommendations that complement medications and create real results—without guesswork or endless theory.
-
You want to become the go-to practitioner in your community who attracts committed patients and builds a thriving practice while learning at your own pace.
Presenters with Years of Clinical Experience

Dr. Asia Muhammad, ND
Dr. Asia Muhammad, ND, is a board-certified Naturopathic Doctor dedicated to bridging science and natural medicine. She earned her Bachelor’s degree in Chemistry and Biology from Middle Tennessee State University and her Doctorate of Naturopathic Medicine from Southwest College of Naturopathic Medicine and Health Sciences (SCNM) in Tempe, Arizona—an accredited medical institution that integrates both naturopathic and conventional medical approaches to healing.
After graduating in 2014, Dr. Asia completed a two-year residency in Integrative Medicine in Arizona, where she gained extensive experience in the evaluation and treatment of chronic diseases. Since then, she has continued her work in private practice, providing personalized, evidence-based care to support long-term wellness.
Her work has been published in leading journals, including Integrative Medicine: A Clinician’s Journal and the Journal of Natural Medicine. She also co-hosted the Amazon Prime award-winning docuseries The Art of Natural Healing, highlighting the power of evidence-based natural therapies.
Dr. Asia integrates clinical nutrition, botanical medicine, and lifestyle interventions to create individualized treatment plans tailored to each patient’s unique needs. A passionate advocate for Integrative Health, she empowers her patients to take an active role in prevention, healing, and sustainable self-care.

Dr. Matthew Cavaiola, ND, MS
Dr. Matthew Cavaiola is a naturopathic physician with 17 years of clinical experience in Functional, nutritional, and herbal medicine. He specializes in cardiometabolic conditions, detoxification, and men’s health.
He received a Bachelor’s Degree in Biology and a Master’s Degree in Human Nutrition from the University of Delaware, a Master's Degree in Acupuncture, and a Doctorate Degree in Naturopathic Medicine. He has been practicing as a Functional and integrative medicine physician for 17 years and was also an adjunct professor at the Sonoran University of Health Sciences and Bastyr University.

Tal Cohen, DAOM, MS
Tal Cohen, DAOM, MS-HNFM is an author and presenter with over 16 years of clinical experience with integrative, nutritional, and Eastern and Western herbal medicine.
He developed multiple Functional and Nutritional medicine programs, lectured nationwide, and is the author of several books and patient guides, including “Treating Pain and Inflammation with Functional Medicine: The Complete Clinical Guide” and “The Complete Guide to Removing Toxins & Improving Your Health.”
Tal completed a Master of Science in Human Nutrition and Functional Medicine and a Doctorate in Acupuncture and Oriental Medicine.

Dr. Chil Khakham, ND, MBA
Dr. Chil is a naturopathic physician with additional training in Functional Medicine, functional endocrinology, and functional blood chemistry.
His education includes a Bachelor of Science, a Master of Business Administration, and a Doctorate in Naturopathic Medicine.
Dr. Chil developed several Functional medicine programs and established and developed several successful brick-and-mortar and virtual practices.

Jessica Knese, MS, CNS
Jess graduated from the University of Colorado with a dual bachelor's degree in Integrative Physiology and Psychology and a Master's of Science in Clinical Nutrition and Integrative Health from Maryland University of Integrative Health. Jess is also a Certified Nutrition Specialist and has been working in several Functional and integrative medicine clinics with primary care providers who implement nutrition into their practice.
The Integrative Health Practitioner Certification Program
December 1st 2025

00
DAYS
00
HOURS
00
MINS
00
SECS
A COMPREHENSIVE PACKAGE
What's Included in the Program...
Register now and receive our comprehensive package and bonuses:
✅ Live Weekly Classes + Recordings — Engage in live training sessions and access all recordings anytime.
✅ Treatment Protocols for Common Conditions — Covering cardiovascular, metabolic, gastrointestinal, endocrine, musculoskeletal, immune, mental health, women's, and geriatric conditions, using evidence-based nutritional, botanical, and lifestyle medicine.
✅ Downloadable PDF Handouts for every class.
✅ Clinical Guides & Patient Resources to apply what you learn in practice.
✅ Private Member Portal with one-year access to all course materials and recordings.
✅ Printable Grocery Lists aligned with recommended nutritional protocols.
✅ Healthy Cooking eBook (Branded for Your Clinic) featuring simple, evidence-based recipes for patient support.
✅ Functional Medicine Phone App (1-Year PRO Access) — Instant access to protocols for hundreds of chronic conditions.
✅ Nursing Continuing Education (20 CEs) — Accepted in 46 out of 50 U.S. states.
✅ Printed Certification of Completion to showcase your new credentials.
✅ Lifetime Listing in Our Providers’ Directory to enhance your professional visibility.
✅Dedicated Phone app with treatment protocols for hundreds of adult and pediatric conditions
Program Cost: $4,500
Healthcare provider scholarship includes a discount of $2,100!
Bringing the price to just $2,400
Apply For Program + ScholarshipFrequently Asked Questions
Who can register to this program?
How long does it takes to get certified?
Why should I register for this program?
What if I cannot attend the 1hr live class every week?
Will I learn about the treatment protocols?
Who is the creator of the Integrative Health Practitioner Program?
I have additional questions. Who can I contact?
Apply For Program + Medical Scholarship
Schedule a short call with an academic advisor
The Integrative Health Practitioner
Certification Program
Starting December 1st 2025

00
DAYS
00
HOURS
00
MINS
00
SECS
